Pediatric Emergency Care is Lacking in America. Some hospitals in the US aren’t fully prepared to treat kids in emergencies. Why is this a big deal?
Pediatric Emergency Care: The Current Situation
Imagine your child breaking their arm while playing soccer, or having a sudden allergic reaction to something they ate. You would rush them to the closest emergency room, right? But here’s the kicker: not all emergency rooms are fully ready to treat kids. Children aren’t just tiny adults; they have unique medical needs and require specialized care.
Hundreds of children are injured or even die each year in the US after being taken to poorly prepared emergency rooms.
The Wall Street Journal found that “only about 14% of emergency departments nationwide have been certified as ready to treat kids, or are children’s hospitals specializing in treating young patients.”
Heartbreaking Stories
You may be wondering, “Why does this matter?” Some children in America, including in South Carolina, have been injured or have tragically passed away because the emergency care they received wasn’t up to par.
Here are a couple of cases:
A three-year-old was suffering a seizure when she was rushed to the hospital. The doctor wanted to install a breathing tube. The breathing tube handed to the doctor by staff was too large for the toddler.
Because a child’s airways are smaller than an adults’, and the breathing tube must be positioned differently, intubating a toddler can be especially tricky for a doctor who does not specialize in pediatrics. Children also lose oxygen more quickly than an adult, so intubation needs to happen fast.
After the doctor could not intubate with the adult tube, he tried multiple times with smaller tubes and failed. The toddler lost too much oxygen and her heart stopped.
CPR was attempted, but once again, staff used adult drug doses. She was finally stabilized but had gone without oxygen for too long. Sadly, she passed away several days later.
Preventable Life Altering Injury
In another case, a 4-year-old went to the ER for stomach pain and vomiting. Emergency staff gave him Tylenol and apple juice. They did not order an x-ray of his bowel until four hours later. They had planned to send him home before the x-ray results even came back!
Once they got the x-ray results, he was rushed to a children’s hospital, where he was diagnosed with intussusception, a crumpled bowel. Doctors who do not specialize in pediatrics will sometimes mistake intussusception in a child with constipation or a stomach virus. If caught early, intussusception is easily cured.
Because it took so long to diagnose him, the boy’s oxygen dropped to a dangerous level, and he went into septic shock. In the operating room, his heart stopped. He ended up needing multiple surgeries on his bowel and lungs. He suffered long-term lung damage, and has been hospitalized several times for pneumonia, caused by the lung damage. (WSJ.com)
These are just a couple of examples: reasons why we need to spread awareness about the importance of pediatric emergency care readiness.
The Pediatric Readiness Project: A Ray of Hope
To tackle this issue, there’s a nationwide effort called the “Pediatric Readiness Project.” This project aims to ensure that every emergency room is prepared to give the best care to children. Hospitals are being evaluated on how well-equipped they are, from having the right-sized medical tools for children to training doctors and nurses to deal with pediatric emergencies.
“Steps that research has shown E.R.s should do to be ready to take proper care of children:
- Doctor coordinator for pediatric emergency care
- Nurse coordinator for pediatric emergency care
- Staff are tested periodically on pediatric care skills, such as resuscitation
- Careful monitoring of quality and safety markers specific to children
- Child-specific protocols, such as identifying abnormal pediatric vital signs
- Written all-hazard disaster plan that accounts for children
- Evidence-based decision support tools available to doctors in real time
- Written agreements for where and when to transfer young patients
- Safety measures, such as only weighing children in kilograms to avoid confusion, and using guides that pre-calculate drug doses
- Stocking child-sized equipment and medications important for children, and training staff on where to find them
Source: Pediatric Readiness in the Emergency Department Checklist produced by the American Academy of Pediatrics, American College of Emergency Physicians, Emergency Nurses Association and Emergency Medical Services for Children Innovation and Improvement Center, 2021.”(WSJ.com)
How Can You Make Sure Your Child is Safe When There’s an Emergency?
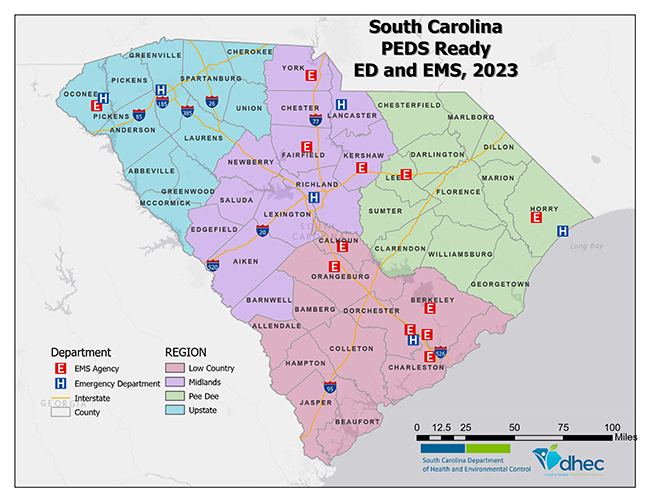
“In 1994, the South Carolina Department of Health and Environmental Control (SCDHEC) obtained federal grant funding to integrate the special treatment needs of pediatric patients into the state’s EMS and hospital systems. This program became the South Carolina EMS for Children (SC EMSC) program.”(dph.sc.gov)
This link will give you information on which South Carolina hospitals have been awarded pediatric-ready certificates. These are hospitals that have voluntarily applied for a certificate.
South Carolina hospitals that specialize in pediatrics along with their websites:
MUSC Shawn Jenkins Children’s Hospital (Charleston) https://locations.musckids.org/sc/charleston/10-mcclennan-banks-drive-fac151utm_source=Yext&utm_medium=Listings&utm_campaign=WebsiteClicksFacility
Prisma Health Children’s Hospital (Columbia) https://prismahealthchildrens.org/locations/hospitals/childrens-hospital-midlands
Prisma Health Children’s Hospital (Greenville) https://prismahealthchildrens.org/locations/hospitals/childrens-hospital-upstate
Shriners Hospital for Children (Greenville) https://www.shrinerschildrens.org/en/locations/greenville
McLeod Children’s Hospital (Florence) https://www.mcleodhealth.org/services/care/childrens-hospital/
Stay Informed: Share this information with your friends and family. Awareness is the first step towards change.
Support Local Hospitals: Find out if your local hospital is a part of the Pediatric Readiness Project. If not, write to the hospital management or local representatives, stressing the importance of pediatric emergency care.
Safety First: Have your children practice safety guidelines in sports, be aware of food allergies, and always require them to wear helmets and seat belts.
Every Child Deserves the Best Care
Every child, whether in The Palmetto State or any other part of America, deserves the best emergency care. By staying informed, supporting the Pediatric Readiness Project, and taking safety precautions, we can all play a part in ensuring a safer future for our children.
Stay safe, stay aware, and remember that every voice can make a difference!
Contact The Law Offices of David L. Hood for a Free Medical Malpractice Consultation
If you, your child, or someone else you care about has suffered because of medical negligence, please schedule your free consultation by calling The Law Offices of David L. Hood at (843) 491-6025 or filling out our brief online contact form.
We know how difficult it can be to deal with the immediate and long-term effects of a serious malpractice-related injury. At The Law Offices of David L. Hood, we work hard to make things simple for you. After a free case evaluation, if we believe we can help you and your family, Medical Malpractice Attorney David L. Hood, co-counsel, and our team of experts will vigorously pursue your case to get you the best result we can achieve. Let us put years of experience to work for you!
*Clients are not liable for any expenses, unless there is a recovery in their case; however, if there is a recovery in their case, clients will be liable for expenses. Attorney’s fees are based on a percentage of the recovery, which will be computed before deducting expenses.